Category Archives: Lean Healthcare w Polsce
Problem solving with 8D report
What is 8D analysis? It is a problem solving method created by U.S. Department of Defense in 80′. The method itself was used by Ford and others automotive companies. It is also used by medical branch, lean healthcare/ lean hospitals.
Analysis is based on 8 easy steps, that lead you to root cause and later to preventive actions. As lean healthcare heads towards improving clinical processes, it’s not only good for understanding problem but also for finding fast solutions and above all corrective actions that REMOVE cause of the problem.
Below you can see description of each step you can follow to:
1D – TEAM
- Establish the team, which will resolve the problem (it could be nurse, cleaner, head of nurse, technician)
- Team should be multidisciplinary, not big for example: 2 to 5 person
2D – PROBLEM DESCRIPTION
- Describe the problem which occured. If you have good description, you will find good solution.
- WHAT is the problem, WHEN does it occure, WHO find it out? Does it concerns 1 patient or all ward?
- You can visualize problem: photos, pictures, movie, how it is, how it should be,
3D – CONTAINMENT ACTIONS
- Containment actions! If you can correct something, DO IT NOW!
- Inform your superior about problem, or medical staff which is involved in this process
- If you note that for example nurse gives patient incorrect drug, SAY IT, consult it with physician now
4D – ROOT CAUSE ANALYSIS
- Find ROOT CAUSE of the problem
- WHAT or WHO made mistake ?
- Answer the questions, for example: Were the procedures followed? Is the medical staff competent, qualified? Is the medications are identified, correctly described?
5D – CORRECTIVE ACTIONS
- Implement CORRECTIVE action, which eliminate root cause of nonconformity
- Determine appropriate ACTIONS, RESPONSIBLE persons, DEADLINE
- It is good, when deadline is always the same length for example: 1 week.
6D – CHECK EFFICIENCY OF CORRECTIVE ACTIONS
- Validate CORRECTIVE ACTIONS. Did it remove cause of problem?
- Is the problem not recurring?
7D – PREVENTIVE ACTIONS
- Implement PREVENTIVE ACTIONS, which will eliminate POTENTIAL root causes of problem
- Check if the problem doesn’t occure in similar processes or actions (analogical)
8D – FINISH ANALYSIS
- Finish problem analysis
- Thank team for commitment in problem solving
You can use also 5WHY method to deeply understand the problem and find root cause.
Safety of clinical processes
On 26 and 27 of November 2015 the 10th National Health Care Forum anniversary had taken place in Katowice. Some of you had the chance to participate in our lecture concerning safety in clinical processes. We talked about how clinical process can be defined (from beginning to end), how to find and calculate risks, and how can it be decreased. I had displayed an abstract of how we can evaluate the risks in clinical processes.
- Define the process, for which you want to evaluate the risks. It could be the main process, for example, process of hospitalization patient in the ward xxx.
- Define beginning and the end of the process, but please remember that patient starts and finish the process. It depends on you whether beginning will be patient enters on the ward or patient’s contact with physician.
- In order to list actions from the process, the best solution is to go to GEMBA (place, where process works, ward) and observe the process.
- When you do the flowchart of your clinical process, you need to take next step and create a team, multidisciplinary team. Organize the meeting with your colleagues from the ward and conduct brainstorm to point all potential failures, that can occure in your clinical process. You can refer to problems that occured in the past. Remember that we are looking for POTENTIAL failures, which have cause for our process.
- After that point, collect and get your problems in order. Now you have to find the root cause of the failures. For this step you can use ISHIKAWA diagram and 5WHY tool.
- While we have all root causes, now we can evaluate our clinical risks. In order to specified objectively the risks, use FMEA method (failure modes and effects analysis).
- Based on factors SEVERITY FAILURE FOR PATIENT, OCCURENCE PROBLEM IN OUR PROCESS, DETECTION we can evaluate the possibility of occurence the our risks, it could be high, medium or low.
- By relying on RPN (Risk Priority Number) we have to take the actions to decrease or eliminate risks. Now we have an action plan, which realization influences on process safety, quality level of medical services, personnel awareness and people commitment.
- For evaluation process the best is involve colleagues for example: physicians, nurses, ward nurses, administration. The more specialist in the team we have, the better brainstorm we can do and risk evaluation is more precised.
- You can conduct risk evaluation while process is implemented or when medical entity is just built. Thanks to that you will find WEAK POINTS IN THE CLINICAL PROCESS which you will eliminate.
I had presented briefly the risk process evaluation ( it concerns every medical process, which you can meet in big and small hospitals, doctor’s office).
Methodology 5S
Order and arrangement at the workplace
Maybe the header doesn’t persuade to get to know the 5S method however, everyday safety and ease of work strongly depends on it. There are lots of activities in a hospital since everone strive to make his or her work done properly. As more patients stay in, it gets more and more difficult to maintain decent workplace. If we consider medical services process from the angle of used supplies, we can simply notice that any arrangement, setup or configuration becomes a repetitive obstacle and preserving workplace ergonomics, adjustment of medical equipment and distance to stocks located in storage facilities isn’t as simple as it should be. The more workplace is arranged and ordered the more we’re able to notice issues elswehere. 5S method has its origins in Japan and is associated as a continuous improvement tool. Widely used in various branches including healthcare.
What to do first?
Method name indicates number of stages that must be followed in order to make it most efficient. Each stage unveils its various meaning.
1S-SEIRI
Selection – it stands for tools selection so that one can perform an action and a perfectly valid process. It is important to remove unnecessary objects. Define frequency for hardware, objects and tools use. If there is any equipment used ver rarely it is likely to place it in a storage facility in order to gain extra space to work.
Another stage is called 2S-SEITON
Systematics – it determines where to place hardware and objects. Each area should be described and pictured because visualization facilitates any kind of work. Convenience and frequency of use are here top-notch factors – the more we use an item the more close it should be located. Thanks to S2 SEITON each item has its own fixed spot and we level time spoiled on looking for it. Furthermore, it gets straightforward to evaluate shortages and execute quick supplies. Another significant component is to outline pathways, doors, room for medical equipment. Particularly important in preparing emergency equipment including specific medications and items (secured dose and amount). If items of a set lay down unordered in a drawer it’s hard to guess if there is something missing. However, using dividers or a shadow boards makes it organized and easy to identify (shadow board is a map of item shapes e.g. shapes cut in a special foam hanged on a wall always display the missing item if it’s not there).
Shadow board is great solution for tool management at workplace. It allows define status of tools and quantity promptly. Shadow board serves for cleaning kit but also for:
- drugs and syringes
- surgical instruments
- emergency tray
- other technical tools
Shadow board allows for keeping order according to 5S methodology. This is visual tool, thanks to medical staff don’t waste time for looking for things. It allows to complete activity in safety way. Clinical processes are specific, because that it is important to use intelligent and relatively cheap solution. Shadow board is tool created to everyday control of emergency tray. Just one look and it is known if tray is completed or not.
3S-SEISO
Clean-up – it’s not only about cleaning up. Systematic cleanup according to hygiene schedule helps to maintain appropriate hygiene along with safety expansion. Cleaning up also means to control in order to identify broken equipment, damaged items, any defected or nonessential conditions that doesn’t fit regulated standard. Criteria of control are composed by ourselves. A person responsible for cleaning up is also assigned to evaluate actual condition and record any aberrations. There’s always a clean-up personnel in a hospital – ward nurses perform activities having enormous impact on clinical process safety. Accurate assessment using 5S method can easily eliminate risky situations which have been always a possible risk to medical personnel or patients e.g. leaking tap in patients bathroom… maybe it’s not a big deal but suppose water drains on the floor and our patient falls. It may cause grievous bodily harm or even death. After getting such a result in our 5S evaluation process a quick preventive reaction is necessary. Each staff member should be responsible for his or her spot.
4S-SEIKETSU
Harmonization – it pertains to above mentioned stages. We define the rules, form standards and maintain both. It is obliged to follow certain duties, schedule and sanitation safety plan. Both law requirements and internal procedures are being developed and this is why it is so important to fit new rules and improve them.
5S-SHITSUKE
Self-discipline – reassures to abide above mentioned stages. It is essential to introduce an evaluation system as an everyday routine. 5S audit should be performed by determined clean-up personnel that’s responsible for order in a workplace. Best results can be acquired when 5S isn’t just required from 1st degree personnel but from all employees including executives. The easiest way is to begin with the first degree personnel, and ending with executives.
PROS?
– safety improvements
– shortening the distance coverage of Staff
– increased staff knowledge
– arrangement among medical records
– appropriate workspace management e.g. storage facility for medications, dressings or equipment items. All above mentioned advantages relate to entities financial liquidity and lower the risk of having medications or equipment with expired date which in fact are producing losses of a hospital
– simple and quick evaluation of occuring action
– higher efficiency and productivity of provided services
5S audit
Methodology 5S is the beginning of long way to improvement with lean healthcare approach in medical unit. There is no patient safety management without well equipped infrastructure and without defined duties and responsibilities at every workplace. 5S implementation is not easy task, but its maintenance is more difficult. It is difficult to convince employees to work according to new rules and standards. Acquisition of new information and change the habits is hard and long term process, but using Kaizen philosophy is easier to reach goals. How after 5S implementation, keep this system in the hospital?

Methodology 5S consist of 5 steps, which are described above. How to conduct daily 5S audits?
It is worth to design checklist in which defined employees will be conduct assessment. Forms should be adequate to each workplace, department and hospital wards. Other aspect will be checked by cleaner, other by technician and medical caretaker.
5S audit form should be divided on 5 parts (5 steps):
- sort
- set in order
- shine
- standardize
- sustain
and days of week, we want to conduct assessment.
Each stage contains questions and aspects which should be followed every day.
Sort is checking workplace if there is no unnecessary things, machines and equipment which could make work more difficult.
Set in order means systematic lay down equipment and other things on defined place. Each machine, wheelchair, USG machine, EKG have own address, so that it is possible to keep order. Things that are used most common are located on hand, in the nearest place.
Shine is everyday activity in each patient room, hospital ward, ward kitchen and warehouses, also it is infrastructure which is used less often.
Standardize allows for conducting 5S audit according to checklist. It is also linked with documentation results of assessment.
Sustain- this point suggests employee take care of own workplace, proposing improvements and observing own surrounding. When problem appears, medical staff or other employee find some lost drug, should inform supervisor and protect place so patient and employee will be safe.
KANBAN system
Ordering stockroom supplies by use of KANBAN cards
It’s a simple stock logistics system and manufacturing management geared towards optimization of information flow and any kind of stock during a process. Basically, it refers to resource management in order to provide necessary quantities always on time, triggered by the KANBAN card and its appropriable indicator signal. When it comes to manufacturing, it was always considered one of the most popular tools to resource management. By minimizing stocking area it enables necessary resources to arrive on time according to formerly placed order. Kanban also bases on a crucial method called pull system. It means that demand of a product is raised in a practical moment with its precise quantity.
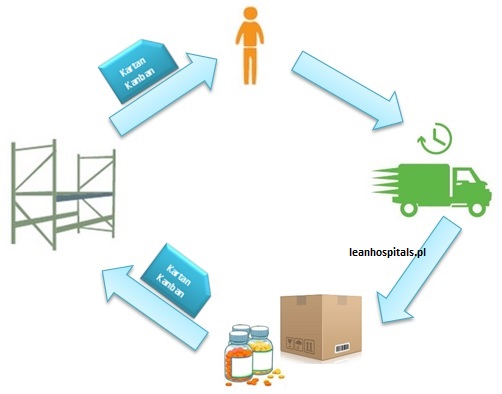
Speaking of management system, it’s completely new to the services area. No analogy to manufacturing makes it extraordinarily responsive towards specific branch. Most present in hospitals storerooms to provide dressings, disposable materials, medical equipment and medications. Under no circumstance should supplies reach their limit. The possible risk can even result in disruption of medical service. In other words, cause patients death or complications. In terms of medical branch, kanban system turns up to work outstandingly in storerooms equipped with disposable materials and medications.
How do we practice this approach?
Within an entirely organized stockroom each material has its assigned location, so called address. Material names are described on a wall, shelves and containers. Quantity is assessed according to current consumption. Minimum stock is crucial to regulate process performance and order supplies to have it received on time:
Due to specificity of medical service and its precariousness, process can turn out to be patchy, our safety stock can vary. Stock minimum can be visualised in various ways – red line on a wall, shelf or special container. Each resource is given a KANBAN card. If one can note minimum stock level indicator the kanban card should be collected and succeeded by placing an order.
Advantages:
- optimum quantity of supplies
- proper storage area management
- no outdated item
- simple visual management
- uninterrupted information flow
There are many advantages but the most important is the continuity of medical process. If stockroom always ensures minimum supplies the safety has its maximum level. All in all, safety of process and medical staff confidence are to reduce risk.
POKA-YOKE
We use it to stave off miscellaneous errors. Japanese engineer Shigeo Shingo is the originator of this method – he accumulated solutions to exclude any sort of mistakes during procedures. In everyday life there are many conveniences of this kind e.g. driving a car, reheating food in microvawe or plugging charger to a socket.
Clinical process vs. risk
Every hospital, which clinical process poses a major risk of mistakes, looking for modern and efficient solution. Poka-yoke in clinical process is very useful method, which prevents errors, adverse events and near misses. Patient which use of medical service want that process will be fast, proficient and without any complication. High safety level depends on qualified personnel and needed infrastructure. If infrastructure is well designed it is error proofing.
Repeated activities let the guards down
Frequently repeated the same or similar activity can lull into a false sense of employee security. Routine could be potentially root of mistakes, it is very important to use well designed medical equipment. So that medical staff can use time for creating value added activities for the patient. Effective poka-yoke shouldn’t lead to wrong output of activity. Poka- yoke solutions are divided into 2 types:
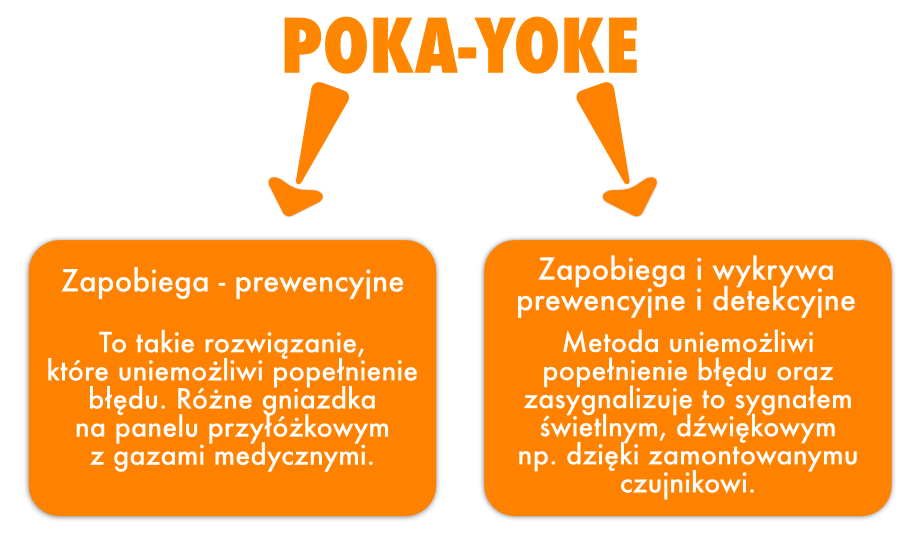
Poka-yoke examples
Medical equipment, machines and clinical processes with poka- yoke secures:
- wrong plug in medical machines
- performance wrong activities in next process stages
- omission activity in clinical process or its realization in wrong order
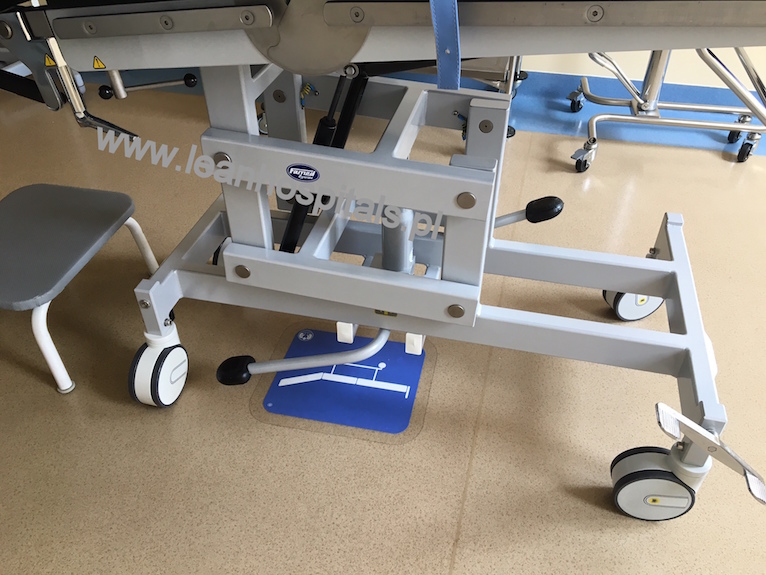
Visual Management
Visual management in healthcare
Visual management is one out of many lean management tools essential to professional fields and also life areas. The purpose of VM are process improvement and defining a perfect procedure.
Basically it’s a concept of simple and intelligible signs e.g. graphics on hospital premises to organize area, monitor work, appliances and equipment in use. It makes simpler to evaluate an actual state, quicken reaction on issues during a process and facilitate communication. Visual management reinforces patients and employees safety because of self-restraint feature. All tools are very obvious and intelligible for its users and allows to standardize procedures and make them much more consistence. One of the elements of visual management are floor markings that determine placement of equipment, appliances, wheelchairs and hospital beds. It may also be defined by light indicators.
By using VM in healthcare facility work standards are ensured because it’s possible to equate actual state with the desired one, and what’s more, evaluate if it’s close to being perfect or detect any aberrations.
Compelling constituent while implementing VM tool is awareness and engagement of staff in favour of safety improvement, standardization and enhancement of work and services quality level. It is recommended to divide this implementation into separate departments. Starting with visual management in medications and medical dressings stockrooms or clean-up personnel and utility rooms or surgery. Competent implementation and awareness of respective staff groups will trigger mutual learning between them.
Examples of visual management tools in health care facility
- illustrating activities of a process
- placement and intermediate storage area e.g. hospital beds, wheelchairs, ultrasound scanner
- determining borders for equipment and appliances
- passing simple statements to a patient or personnel – light indicating access to an office
- designating passageway and isolation passageways that cannot cross each other
- organizing workspace and assigning appliances to its stationary place – 5S tool
- using message signs
- organizing documentation
- differentiating job positions by uniform colour
- increasing work and services quality level
- reinforcing safety of personnel and patients
VM improves processes by direct and indirect actions that have huge impact on health and life of patient and personnel safety at work.
In the age of usage of infographics, posters and statements presented in a pictorial form, are organizations able to adequately manage risks, which occur in the processes, not only clinical but also supportive?
This is possible in every medical institution. As the manufacturing industry strives to minimize issues and downtimes as the medical industry is striving to reduce the occurrence of medical adverse events. Often medical incidents, adverse events are caused by ignorance, lack of qualifications or non-adherence to follow procedures. An important element is documenting of incidents, analyzing them and finding the source of the problem. An electronic public health service platform, which allows public administration authority and citizens gather, analyze, and share resources about medical events may be helpful. The purpose of the platform is to exchange information, better crisis management and statistics as well as improvement of quality of provided services. This project was called P1 System [Kaczorowska-Kossowska 2013].
Some statements may be simplified and presented in a visualized form. Visual management is not introduction of graphical information for the presentation itself. The objective of visual management is to control process and to assist in risk management. Not always examples of image content will qualify as an example of visual management.
The purpose of usage of visual management is to allow for indication of deviations, which occur in the process and then quick reaction to minimize or compensate them. Another objective is to present the current situation of the process, it may be a work schedule, hygiene plan for a specific hospital ward or matrix of competence which indicate the persons which may replace specialists during their absence.
The forms of visual management that can be encountered in medical institutions include:
- Boards with admission dates
- Signs that point the way
- Signs such as “caution, wet floor “
- Lights – ANDONS – above the door of the doctor’s office which inform the patient about the possibility of entering the office
- Instructions for hand washing in the form of graphics or photos
- Procedures in form of flowcharts
- Graphics defining security and ergonomics such as no smoking, quiet please, please turn off mobile phones in hospital registration
Performance based on quality standards also allows for detection of issues and incompatibilities, which should be removed and also allow employees and managers to gain knowledge. Detection of incompatibilities and observations will allow to conduction of training and improving the qualifications of employees. Incompatibilities may apply to medical documentation, protection of personal data and ignorance of staff regarding procedures. Opportunity is to increase staff awareness of the importance of quality in medical services. Performing internal audits and reporting increases the safety of patients and employees. Work becomes standardized and because of visual management elements such as process maps, both the patient and the employee can determine the next steps or stages of the process. Work in the medical industry is variable, patients change, their conditions, afflictions, law or range of reimbursed services. The institution to survive has to adapt to these changes otherwise it will become an uncompetitive institution with an average opinion. The use of procedures, standards and quality principles wouldn’t be easy without effective communication. The use of intranet, information boards or web page improves communication and increases knowledge and awareness of employees. Regular publication of educational materials demonstrates commitment not only to the patient’s treatment process while patient stays in the institution but also in teaching and raising awareness about healthy living and civilization diseases of the local community.
In order to control the process through visualization, it is important to update the data at a specified frequency. This will allow each participant in the process to know its status and next objectives. It is also motivation function because it encourages employees to follow the indicated graphics and to perceive situations in which the process contains issues.
Visual management in health care facility





Visual management in hospital (ASQ case study)
Visual Management is a very useful tool to manage space by using visual signs. Thanks to VM it is possible to run unflawed process and report its certain stages – including abberrations or errors – to provide quick prevention. Floor signs make very good example of informing about assigned spots for locating equipment or borderlines – floor tape – to permanently locate each item. VM includes flowcharts to simply depict a process, its necessary resources, results and personnel responsible for accomplish exact stage or complete process.
Polish Dialysis Center Employees Use Visual Management to Increase Safety, Improve Organization of Medical Facility
by Katarzyna Złotowska and Adam Wise
The Regional Nephrology Centre (RNC) in Poland uses efficient and effective methods of lean philosophy to ensure patient safety and a high-quality level of medical services.
The RNC was experiencing problems related to workspace organization, use of utility rooms, and treatment space shared among patients.
Staff used visual management (VM) lean methods such as 5S, gemba, and kaizen to improve organization and efficiency of hospital space. At a Glance .
Clear order and organization of tools, equipment, and personnel are crucial components for businesses to ensure daily operations run smoothly and efficiently. These components are even more critical in medical facilities where staff is challenged with providing safe and effective care space, especially in life-and-death scenarios. At the Regional Nephrology Centre (RNC) in Poland, disorder in utility rooms caused cramping of space and confusion among staff while seeking treatment devices for patients suffering from chronic kidney disease and other ailments. Acknowledging their facility had plenty of room for improvement in the utilization and organization of facility space, RNC leaders sought to improve management of their equipment to increase patient safety and work quality of medical staff.
About Regional Nephrology Centre
The Regional Nephrology Centre (RNC) is a dialysis medical center headquartered in Poland. The RNC provides complex treatment and care of patients with chronic kidney disease and diabetes. The RNC has two locations. The RNC employs 52 individuals, including medical staff, specialists, and managers. Every year, the RNC performs 16,000 dialysis sessions, about 300 hospitalizations, and 1,200 medical counsels in medical nephrology and diabetics practice.
Visualizing the Future of Patient Care at RNC
By improving order and organization, RNC staff would not only address accessibility and safety concerns for staff and patients, it also would affect the bottom line as it decreased the possibility of damage to medical devices by not moving equipment from place to place. But in April 2014, standards were not followed by employees and equipment was misplaced, creating delays and problems for nurses and other medical staff as time was wasted—critical time that should have been spent with patients. “In rooms were things that shouldn’t have been there,” said Katarzyna Zlotowska, lean hospitals engineer at the RNC to improve clinical processes and supervise quality management systems. “Every time it was another room, another place; nurses wasting their time looking for equipment. Even some devices were used in a wrong way such as scale chairs being used as chair.”
Disorder not only created confusion among staff members, but also potential obstacles during times of emergency when patients would need quick and timely transport through or out of the facility. “There wasn’t any flowchart, visual procedure, or instructions for how to proceed with a wheelchair, a bed unit, or utility tool, or where they should be placed,” Zlotowska said. “There were only non documented, verbal instructions.”
Visual management (VM) is a lean management tool used in many industries as well as in typical life. The main purpose of VM is to improve processes and define how processes should proceed through visualization. It relies on pictures, graphs, sounds, and visual signals, that if properly used, can organize one’s work space, increase efficiency of a room’s arrangement, and provide precise rules on a space’s purpose.
This communication technique brings self-control around the worksite through standardization and continuity of action. Using VM in hospitals ensures specific work standards by comparing current state with future state through medical process flowcharts, process maps, and other means, creating an opportunity to evaluate if a specific current state is correct, or if there are mistakes or aberrations. VM makes work easier for hospital staff while increasing patient safety
Quality Journey
The important element during implementation of this tool was the staff’s awareness and commitment toward improving safety, standardization, and increasing the quality level of work and services. Implementation of VM began April 28, 2014, starting with the storerooms and then the utility treatment rooms. The implementation was divided into individual work units (e.g., drug storehouse, utility rooms). The first month was dedicated to analyzing the possibilities, determining the usefulness of specific assets, and then training individuals on the visual management and 5S methodology. This was conducted in less than one month.
In May and June, ward nurses and other medical staff participated in recognizing new methods. Staff had many questions and new ideas on how VM could be used in the RNC. Then in June and July, new methods were practiced and opinions were shared. Employees were very excited and curious about the effects of VM
The major milestone took place on July 15. During a brainstorming session among the project group, ambitious and practical ideas to improve work and equipment flow were offered. The next step was to design graphs identifying specific place-addresses dedicated for equipment, medical devices, medical bed units, and tables.
Upon confirmation of the lean hospitals engineer and RNC manager, the graphs were printed. Once a producer was chosen and samples accepted that were resistant to chemicals and antiseptic fluids, the signs were printed. The final milestone included implementation of new rules. After several meetings and tests, locations were chosen and items put into order with new rules being obeyed. This project involved multiple personnel, including nurses, doctors, and managers; those who felt changes could start from the “employer lever.”
During VM implementation, the awareness level of each staff division is critical, as employees can eventually take their training and use it to learn from their co-workers and their processes. At RNC this initial process began in utility rooms and spaces where medical equipment was placed.
The following are examples of practical use of VM tools that were used in the hospital:
- Visualizing process activities
- Defining storage areas for medical beds, wheelchairs, and diagnostic equipment
- Delineating places for equipment and devices
- Conveying simple communications for patients and staff
- Defining safety pathways
- Using information signs, including flowcharts, and standardizing colors of cleaning equipment, including trash cans and dusters (red for use in cleaning operation room, blue for cleaning patient beds)
- Document organization, including numbering files, separating by type using colors, and loose-leaf binders
- Easily distinguishing staff based on uniform color
Previously at the RNC staff wore colored uniforms, but they were not detailed and divided according to type and place of work processes using flowcharts—saved time while making work simple and more transparent. The flowchart informs the reader what specific step they are in, how they should continue, what documents should be used for what work, and when the process is finished.
See Figure 2 (available in pdf format) for an example flowchart of process treatment of hyperparathyroidism for dialyzed patients. This flowchart is placed directly in the treatment room so all medical personnel can follow every step to maintain standardization and decrease mistakes. Every step is easily readable, and every operation has an owner responsible for it.
VM improves processes directly (better information flow, transparent steps to avoid one step or more, no risk of confusing the order of steps, provides standardization, shorter lead time) and indirectly (patient health, improving staff safety).
During the first step of improvement—possibilities analysis—stakeholders discussed their ideas, identified which places could be improved and better organized, and showed examples of VS from other countries. The stakeholders included ward nurses and managers. After a brainstorm with medical staff, the following were the planned steps of implementation and improvement:
- Analysis of possibilities and places where VM could be used, conducted by a lean specialist with ward nurses
- Preliminary training for ward nurses with practical samples and examples
- Practical training (workshop) conducted in utility rooms (gemba)
- Brainstorming, collaborative analysis, and setting out possible changes
- Design the signs and create them
- Implement changes and standardize methods
It was time for the lean specialist to analyze possibilities by discussing with management available resources, quality policies, mission, vision, and customer focus. Then, the team defined first-step processes that should be improved while inciting feedback from ward nurses and other medical staff.
Preliminary training showed the possibilities of visual management. Personnel acquainted with the lean philosophy of VM, definitions, and hospital examples were showed how to conduct 5S analysis (a Japanese system used to create a workplace suited for visual control and lean production).
5S
Practical training included covering knowledge of processes and providing awareness of processes impacting patient safety. Using the gemba ideology of going to the scene, trainees went to four utility rooms, and first using 5S methodology, sorted the rooms, defined what equipment and tools were needed, removed items that provided no function for the place, and divided resources for every utility room to avoid useless movements, transportation, and stock.
After the workshop, personnel had more ideas regarding implementing very practical solutions. Space in utility rooms was defined and some storage equipment updated, according to standards. Rooms were rearranged for better space exploitation.
Sign creation was important and difficult. Images were designed with the cooperation of a graphic designer, but the work was at times difficult because of shapes of signs, color decisions, defining details, etc. The signs had to be printed on special vinyl/plastic material resistant to disinfection fluids for floors, frequent cleaning, and good grip. Once the signs were printed, all stakeholders were involved in implementation of changes.
Introducing staff to the idea of VM through short, practical workshops made the team aware of the improvement project’s main purpose. Ward nurses and other medical staff noticed that upon VM implementation, their work became easier while each piece of equipment had its specific, safe storage place. The entire team knew how to handle the tools and where they should be placed.
Results
After implementation of visual management tools in utility rooms and patient spaces, workplace organization has increased in many positive ways.
Ward nurses have sorted things out. Thanks to 5S methodology, personnel created handy places for storing minimal quantities of critical items (fluids, cleaners, small buckets, wipers, etc.) to execute their work. Resources needed to complete their work are now in the nearest available space, so there’s no sign of any of the seven wastes (transportation, inventory, motion, over-processing, waiting, over-production, and defects).
Because equipment now has its own, specific place for housing, risk of breakage has decreased by about 50 percent (previously it usually happened about one time per quarter). Also, patient and employee safety has increased since all standards and requirements are being followed and pathway spaces are passable.
There is no potential injury risk to individuals (e.g., patients stumbling over wrongly placed equipment, patient and personnel infections) because the organization eliminated the causes of potential nonconformities. The risk decreased by about 70 percent. Due to visual management, monthly costs for detergents, mops, and other cleaning equipment decreased about 40 percent.
Thanks to 5S, there are no out-of-stock detergents or medical equipment. Because everything now has its own place, ordering logistics are simpler. The ability to track inventory is much easier, so staff can order only the needed quantity, avoiding excesses and wasted storage space. Also, the time needed to prepare an order has decreased in half. Now nurses go to a utility room, conduct their count, and then order.
As a result, RNC has made progress with visual management and placed vital equipment in effective places. Safety and awareness has increased dramatically; personnel feel like “co-authors” of new changes and improvement, which has been inspirational for all employees.
More info about VM of American Society for Quality (ASQ) case study. READ THE ARTICLE
Spaghetti Diagram
Spaghetti plot is a professional tool used to analyze current process flow. It is aimed at creating a visualization of worker’s movement and the material flow within a process in order to present the current waste and problems.
To create a spaghetti plot analysis it is important to
- Select the process that must be optimised.
- Get to know the individual steps of the process and create a simple flowchart.
- Choose employee or position, that will be observed.
- Prepare a sheet of paper and a pencil and some sticky notes.
- Keep an eye of the worker and draw the path he repeatedly walks. If some activities turn out to be incomprehensible it is necessary to ask some questions to the participants of such a process.
- During the process observation all muda (waste) concerned with lean healthcare such as waiting, errors or superfluous transport should be marked.
Analysis can be done in a specified time period which may be shorter than the shift duration – often determined as 8h.
All marked movement of a worker needs to be analyzed in the next step to find any bottlenecks or tasks which were the main waste to lean healthcare e.g. excessive activities or transport, waiting and errors. The aim is to introduce updates and solutions that would eliminate or minimise the located problem and waist.
What should one pay attention to while observing and generating solutions with use of spaghetti plot?
- collect feedback from employees
- collect feedback from management regarding current issues and planned rearrangement in the process
- take workplace health and safety into account
- take into account all legal requirements and regulations
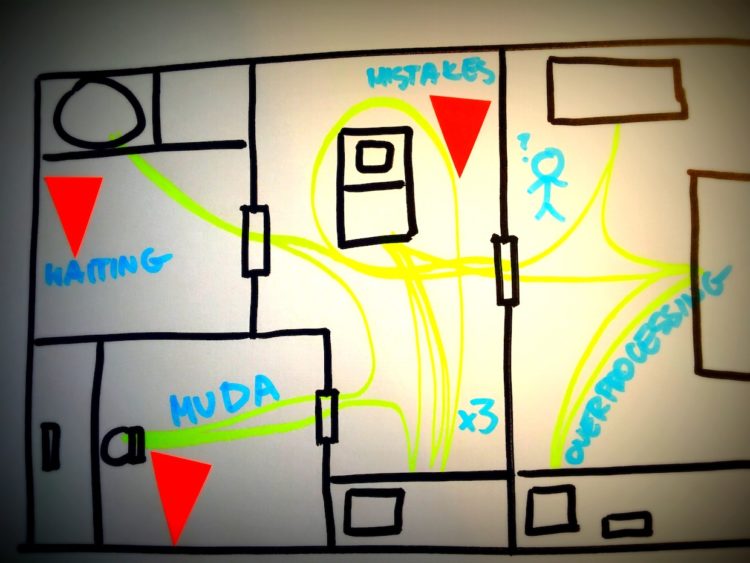
Results
After carrying out analysis and proposing solutions it comes time to take action and implement created solutions in the process. This should be a smooth transition from analysis to action stage – implementation without waiting as this might generate new changes in the process. The longer it takes to implement proposed changes the greater the risk that they will not fit to current process that may suddenly change. A very important issue is the engagement of operative employees in creating changes and collecting comments about their “dream” workplace. Lean healthcare philosophy concentrates on person and its approach to work. Despite good analysis and rapid implementation of improvements, the project may not work out because employees wont adapt to new adjustments. Approach to such a technique should be strategic, taking into account actual needs and ideas of staff by allowing them to actively participate in the analysis and improvements. Joint decision concerning a process will result in partial responsibility that lays on employees for their work and greater efficiency of implemented changes.
It’s a quick and cheap method that allows to capture current problems of a process. Project success, that is, implementation of the proposed improvements will depend on engagement of personnel and collecting detailed information about the process.
About Lean-hospitals
Lean Hospitals is a lean management philosophy which originates from lean manufacturing and lean management. Strongly associated with efficient approach towards clinical processes management. Initially used in production but afterwards it became popular in medical services. Today determined as lean hospitals it is concerned as lean management of hospital (every medical unit). Why did healthcare management considered methods we mentioned? It’s because simplicity involves cheap management tools introducing time and financial savings (eliminates waste).
Pros of this technique:
- increases safety of patients and staff
- simplifies clinical processes
- shortens hospital stay
- rationalise work of medical staff
- reduces costs of medical services and functions in medical units
- boosts business efficiency
Stosowanie narzędzi szczupłego zarządzania pozwala na lepszą współpracę zespołu medycznego. Poszczególne narzędzia można stosować do wybranych procesów, niekoniecznie kompleksowo.
What do we improve?
- shortening distance made by nurses or ward nurses during activities like administering medications or changing beddin
- speeding up information flow amid reception desk, patient, family and physician
- support exact order of ward, surgery, reception desk, utility rooms
- unify and simplify instruments sterilization process
- reduce storage space of dressings and medications. Maintain financial liquidity.
Above mentioned improvements are few out of many that we can frequently observe in hospitals around UK, United States or Japan. Lean hospitals is a completely new approach and its derivative techniques originating in todays production can easily evoke doubts. In contrast, it may give rise of rewarding benefits creating another dimension by way of treatment and medical process management.
Kaizen – how to reinfuse the change in patient life?
Japanese philosophy of small steps can trigger in employees desire of implementing changes and actively engage people to improving clinical processes. This also influences on patient and their motivation. Gathering ideas from employees is one thing, implementing solution and maintaining is difficult task is another thing, but possible to realize.
While patient sees his bad test results is scared and doesn’t know what to do. As Milosz Brzezinski writes “there is a tendency for expire the emotions, so after some time determination for obey difficult rules comes down. The mind doesn’t have his own way for long-term sustaining decisions. That’s why is better to show patient, that something is easier energy-related, for example: closer is go to the greengrocer’s shop that chemist’s. If somebody has to walk everyday, it would be easier with shoes lay down next to the bed; then patient shoe and will be easier to get out home(…) if somebody cannot mobilize for 20 minutes running, should focus on any walk” Miłosz Brzeziński, Puls Medycyny nr 6, kwiecień 2016.
If you want to implement Kaizen in your company- hospital, outpatient clinic or other medical unit, it is good start from learn about that, collect some practical examples from other hospitals, benchamrking. Mainly, implementing kaizen has no sense, if it’s forced, because kaizen approach is a continuous process. It is not a project, which as finished you can summarize and collect results. Once well implemented philosophy kaizen could be acceleration for continuous improvement and succeeding lean healthcare tools. If employees- physicians, nurses, technicians, medical caretaker and top management actively and permanently engage in change process, it will be success for entire hospital.
Proposing ideas, which can inspire other shouldn’t be intrude (some corporation force employees to report for example minimum 5 ideas/person/quarter, as KPI for each department). This is not compatible with Kaizen philosophy. I disagree with this approach. Usually, ideas comes spontaneously, not imposed, that’s why great ideas were made in different situation, not working at desk but meeting with people in gemba.
The process of reporting ideas in medical unit should be standarized, described, the best in visual way and public for all employees. The possibilities of reporting ideas shouldn’t be divided into group. Every of employee should have the same possibility to report improvement- if it is nurse or medical staff, they also can report some idea for administration department and conversely.
After message of optimization clinical process or other, team (the best way is to have top management as main nurse, unit manager and worker) read all ideas and giving them level of priority. Every idea should be appreciated, rest which will be implement into real life should be particularly awarded. Medical staff should feel appreciated and motivated for further actions.
How often should we organize summarize for reported ideas? Well, the findings can be tracked online, summarize meeting can be organize quarterly or half-yearly. This meeting is rather gathering data and giving feedback than people motivating. Motivation should be conducted complete year, day by day.
Advantages:
- Medical staff and administration is valuable source of information and ideas for hospital.
- Improvement communication process in organization.
- Increase employee engagement- also this is TWI element.
- Improvement patient safety.
- Knowing by employees problem solving tools.
- Eliminating muda.
- Descrease costs of hospital functioning.
- Improvement patient care quality.
- Prevention of infection.
Rules:
- Each, reported idea is valuable and should be discussed by kaizen team. Think about how to do it, rather than why can’t we do it.
- Practise japan rule of small steps. It’s better improve something about 30% than doing nothing. There is no possibility to create ideal process first time.
- Kaizen team should systematically browse ideas.
- Every reported idea is appreciated. Internal employee motivation should be fulfilled.
- Kaizen is never ending story- process.
In conclusion, kaizen is first step to work organization according to lean healthcare approach. Solve the problems, without blaming.
